It’s no secret that US human service providers across the nation are having difficulty hiring enough staff. What’s causing this shortage and what can be done about it?
It’s not a simple answer.
While some people are convinced that the main reason jobs are going unfilled is due to the pandemic-related extension of unemployment benefits and additional payments offered by Federal and State governments, Patrick Watson of Forbes disagrees.
In a recent article Watson states, “If, in fact, benefits are what’s keeping people from working, labor shortages should ease in the states that end them. I think there’s more to the story, though. This problem was already there before those extra benefits. It’s more the result of larger trends that aren’t stopping. If anything, they are getting worse.”
The economy emerging from the pandemic also looks different from the one that preceded it. Demand is higher in some job sectors and lower in others. Workers have left jobs in some industries for roles that are less exposed to the coronavirus, or offer better work-life balance. According to the US Department of Labor, in the United States, a record 4 million people quit their jobs in April. A recent survey of more than 16,200 employees globally found that more than half would consider leaving their job if they weren’t offered enough flexibility on where and when they work.
Structural Change.
“This is a time of flux,” Erica Groshen, who served as commissioner of the US Bureau of Labor Statistics from 2013 to 2017 told CNN recently. “It’s not so much that it’s an overall labor shortage, as a time of structural changes for the economy.”
Pam Fields, CEO of Assistive Technology Training Center (ATECH), takes a longer view based on her experience. Fields says, “the real issue – and we knew it was coming – is that there’s not enough people born today to cover the caretaking needs of the nation and the world.”
According to the US Chamber of Commerce’s recent reporting, since 1977, the working population (those aged 15–64) has stopped growing and is starting to shrink (see chart).
Furthermore, when you look at workers by industry, the educational and health services fields have had an even more difficult time in finding workers. In the Worker Availability information produced by the US Chamber of Commerce, the number of workers available to work compared to the number of job openings in the health services field is under 1:1 — meaning that there are already fewer than 1 workers available to fill open positions.
No more worker surplus means employers don’t get the luxury of picking from multiple candidates.
Retention rates for the human services industry have always been an issue, and given the current state of the employment market, it’s likely to get worse.
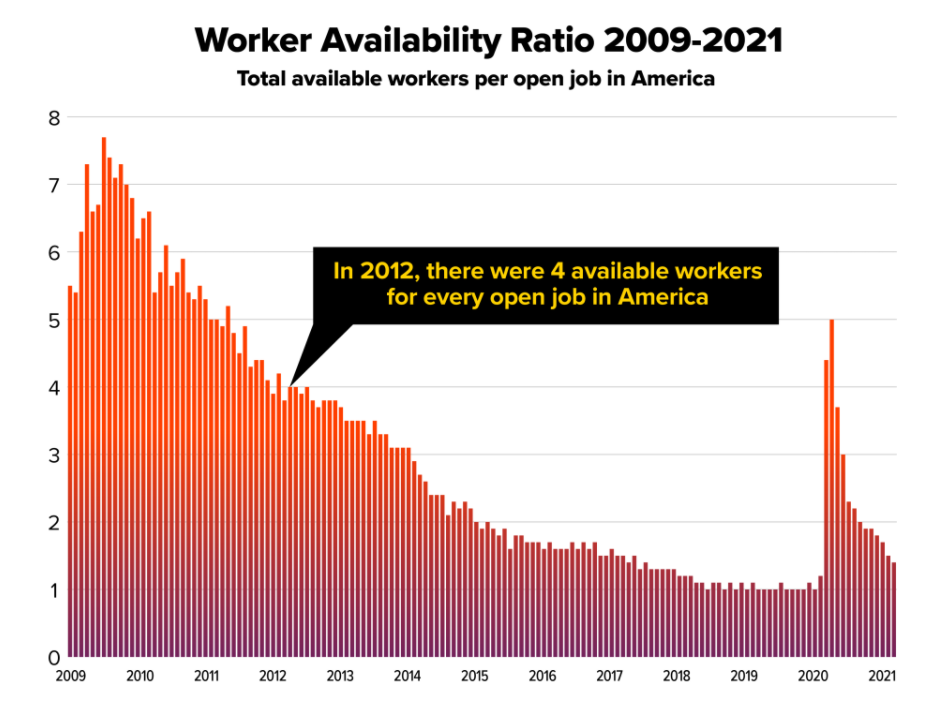
Source: US Chamber of Commerce
Source: US Chamber of Commerce
So what are employers doing about it?
Many are offering more money as an incentive to hire, and to keep, employees.
As Pam Fields says, “they say that part of the reason we have retention problems is the level of salary, and it is true that when the minimum wage and wages in our industry were equal in the past, people would choose to go work at McDonalds and flip burgers for the same wage as opposed to doing the harder work of personal care that can involve things like changing adult undergarments and providing nutrition through feeding tubes. People will naturally gravitate to easier work for the same pay.”
Fields goes on to outline the recent changes in pay for direct care workers.
“We worked hard with the state of Connecticut in the past to put in a wage differential and a few years ago when the minimum wage was just over $11, they (the State of CT) moved our staff to $14.75 per hour, which gave us almost a 3% wage differential. Right after this, they passed a $15.00 minimum wage hike for everyone. This again would have placed us on the same playing field as everyone else with minimum wage. But, this year the Governor just signed an agreement so that as of July 1, all of our direct care staff will go up to $16.50, next year they will go up to $17.25. If in the year following, they increased the starting wage to $18.00, this would get us back to a $3 differential between us and minimum wage.”
Despite the raise in pay and the concerted efforts by the State to maintain the wage differential, the paucity of workers must still be addressed.
Technology: A Critical Solution.
“One of the things that we have seen as we work with assistive technology is that there are opportunities to use these tools to provide remote services, reducing the dependence on human support. For example, if you have a staffing crisis, you can have someone jump in remotely to assist staff that are in-person. If an in-person staff member of a group home needs to leave their group to help someone having a problem or to take care of a personal care need, another staff member could use the remote technology to assist. The remote staff could log on electronically and engage the group virtually so the group continues to be monitored and stays safe, while the in-person team member takes care of the situation at hand. This provides eyes-on monitoring of the residents at all times, even if it’s via remote technology.”
ATECH members are utilizing the latest innovations in smart-home assistive technologies that are proving to be a practical application to addressing the staffing crisis. With mandated staffing levels, Fields is sensitive to the needs of the direct care providers.
“People can tell us and mandate us to have the right staffing levels, and we do everything we can to get there, but when the staff aren’t available, or if an emergency happens, it’s good to have a back up.” Fields adds “in addition, weather is frequently a consideration in getting staff to their work location, and can cause a sudden staffing crisis of its own.”
“We can have a weather emergency like a blizzard or a hurricane where the staff just can’t get to where they need to be on their regular schedule. We’ve had staff who have had to sleep over at one of our group homes for three or four days because of a weather emergency in the past. Having assistive technology in place would allow someone to assist virtually and give the in-person staff a break to sleep for a few hours or shower or care for themselves. The remote staff would have eyes-on the residents and could reach the in-person staff in case they were needed immediately.”
Improving The Quality of Care.
In addition to offering providers a back-up in case of a sudden crisis, the same assistive technology can also be used interactively to engage group home residents. Technology is available that can be accessed via a television screen, showing the person on the other side in a large format, making them easily visible to the residents. The camera can also expand to encompass a large room. If someone should get up and start walking around the room, the camera expands to take in a larger space and keep them on camera. The remote staff can clearly see everything happening in the room, and can also interact with those in the room.
The technology is also easy to use and access. A simple voice command connects the group home to a remote staff member via a preloaded contact list. Additional features allow users on both sides of the portal to engage in activities together, like watching a video, or reading together.
“In addition to assisting with staffing, the use of assistive technology also promotes a better quality of life for people living with disabilities, in ways we could never even have imagined just 5 years ago,” Fields adds.
Next Steps: Learn More about Assistive Technology & Labor Needs.
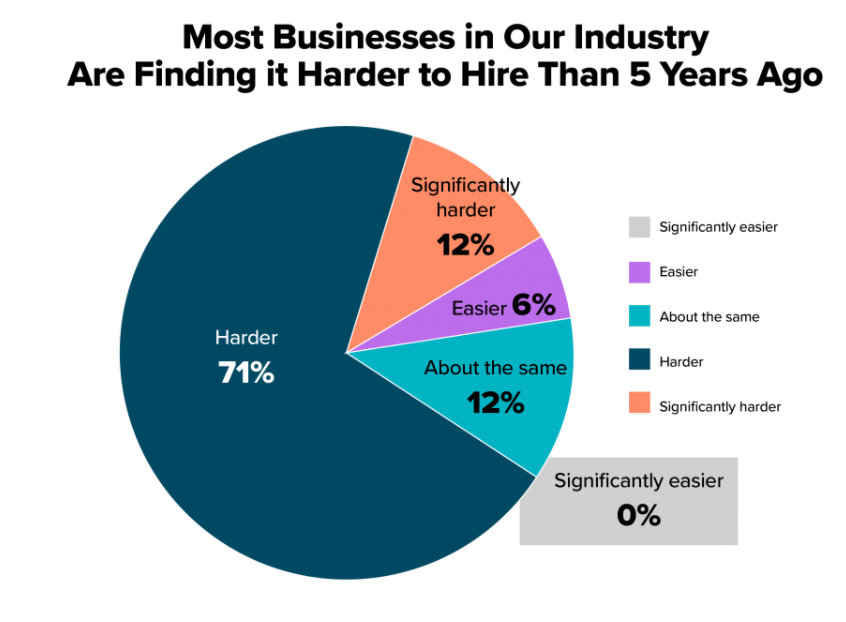
The widespread challenge facing our industry right now is the inability to hire the qualified workers needed. When businesses do not have enough employees, they may be forced to turn down jobs, reduce hours, scale down their operations, and in the worst cases, permanently close. The latest data from the US Chamber of Commerce surveys reveal a national economic crisis that is getting steadily worse.
Pam Fields offers a pragmatic outlook. “I don’t think the staff shortage is fixable due to the fact that there are simply not enough people. In the future, I think we will need a hybrid system. We are going to have to have a system that combines in-person supports and remote assistive technology supports for most living arrangements. However, there are some situations, like severe behaviors or complex medical needs, where eyes-on and hands-on staff are required. Those situations wouldn’t work for a hybrid system. But I would guess that at least 50% of the people receiving supports, if not more, would be able to function very well with a hybrid system in place. I think that assistive technology is the key; there’s no one answer, but assistive tech is a big piece of the pie.”
To learn more about Assistive Technology and Membership in ATECH, contact us.
For more timely articles on Assistive Technology, visit our News & Events page.

